Effective October 1, 2012, the
Affordable Care Act mandated that health plans begin the process of adopting
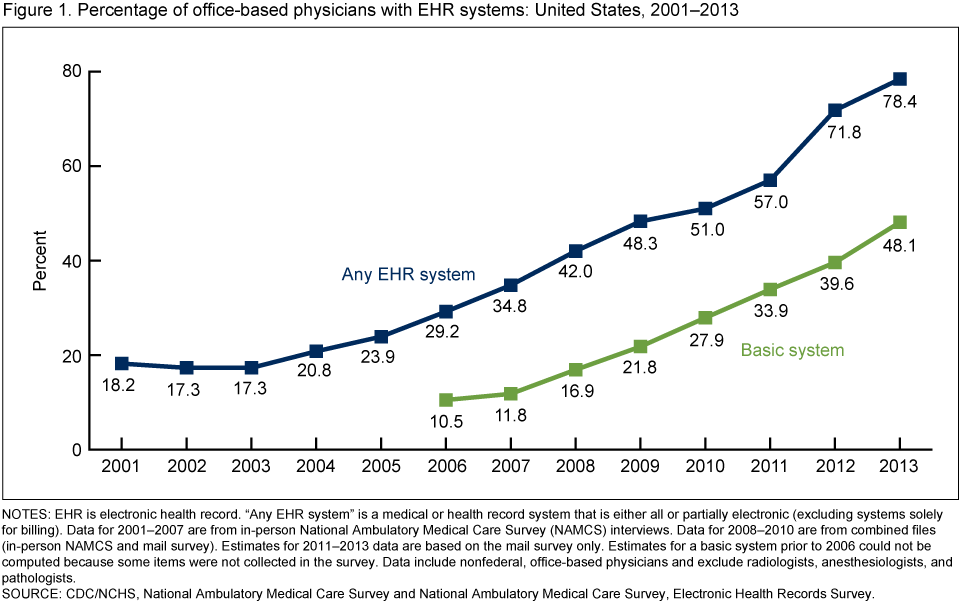
systems for the electronic exchange of health information. From 2006 to 2013,
the adoption of basic Electronic Medical Record systems by office-based
physicians increased by 37% according to a national survey carried out by the
Center for Disease Control’s National Center for Health Statistics.
The pros and cons of EMRs are
varied; some physicians say that implementing Electronic Health Record (EHR)
Systems is costly, time consuming, and disrupts the doctor-patient
relationship. Others maintain that once providers adjust and incorporate EMRs
into their daily workflow, they will reduce paperwork, cut costs, and improve
the way we care for patients. Regardless of complaints about EHR systems,
physicians and hospitals are adopting them, and it is time we worked to improve
their sustainability and efficacy within the health space.
Challenges facing EHR systems must
be addressed if meaningful use standards are to be met and patients are to
benefit. First, we must find ways to increase patient trust in the security of
their health information. If individuals do not believe that their medical
records are safe, they will not be motivated to access or share them. Related
to this, patients must be educated in all of the ways they can use their EHR,
whether that be through sharing their information to further research, tracking
personal health goal progress, receiving clinical reminders, or asking
questions through patient portals. EHR systems do nothing if patients do not
take advantage of their expansive capabilities to connect them with their
physicians and their health information.
Physician input is integral in
determining ways in which EHRs can be more clinically useful. Physician
complaints of EHRs include difficulty taking notes on patient concerns, a
confusing checkbox system, and an overall non-user friendly interface. Though
the platforms for EHR systems may be successful in transferring and storing
records, the way EHRs are used in daily appointments needs to be re-assessed.
Finally, EHR data input systems
must be revamped so that personalized health planning is the fundamental
backbone of the EHR. Patient goals and questions about their health should be
some of the first things a physician sees upon opening the EMR, and the
priority to address during the appointment. Inputting this information should
fit seamlessly into the clinical workflow in order to avoid one of the most
common complains of electronic health record systems; that they reduce the
clinical encounter to a physician typing into a computer.
While
Accountable Care Organizations continue to form and EHR systems are
consolidated and improved, hospitals and health systems should set Health
Information Technology goals that continue to address the major current issues
with EHRs. The potential for positive impact of the EHR in our research,
patient appointments, and overall health system in the future highlights the
need to fix problems with the technology as soon as possible.
Caroline Meade, is a senior at Duke University and a research intern at Duke’s Center for Research on Personalized Health Care.

No comments:
Post a Comment